When you’re in treatment, systems stop being abstract.
Between 2020 and 2025, I depended on patient portals to navigate care. At MD Anderson, the portal was indispensable. Appointments, lab results, imaging, facility updates—everything moved through a single system. My oncologists, radiologists, and care teams across the campus all worked from the same information. That continuity mattered. It meant I didn’t have to reintroduce myself at every step or worry that something important had been missed.
At Texas Oncology, the experience was different. A different portal. A different workflow. A different system altogether.
Neither was optional. Neither was something I chose. They were requirements necessary for compliance, coordination, and care.
The real challenge wasn’t learning how to use them. It was realizing that they didn’t communicate with one another.
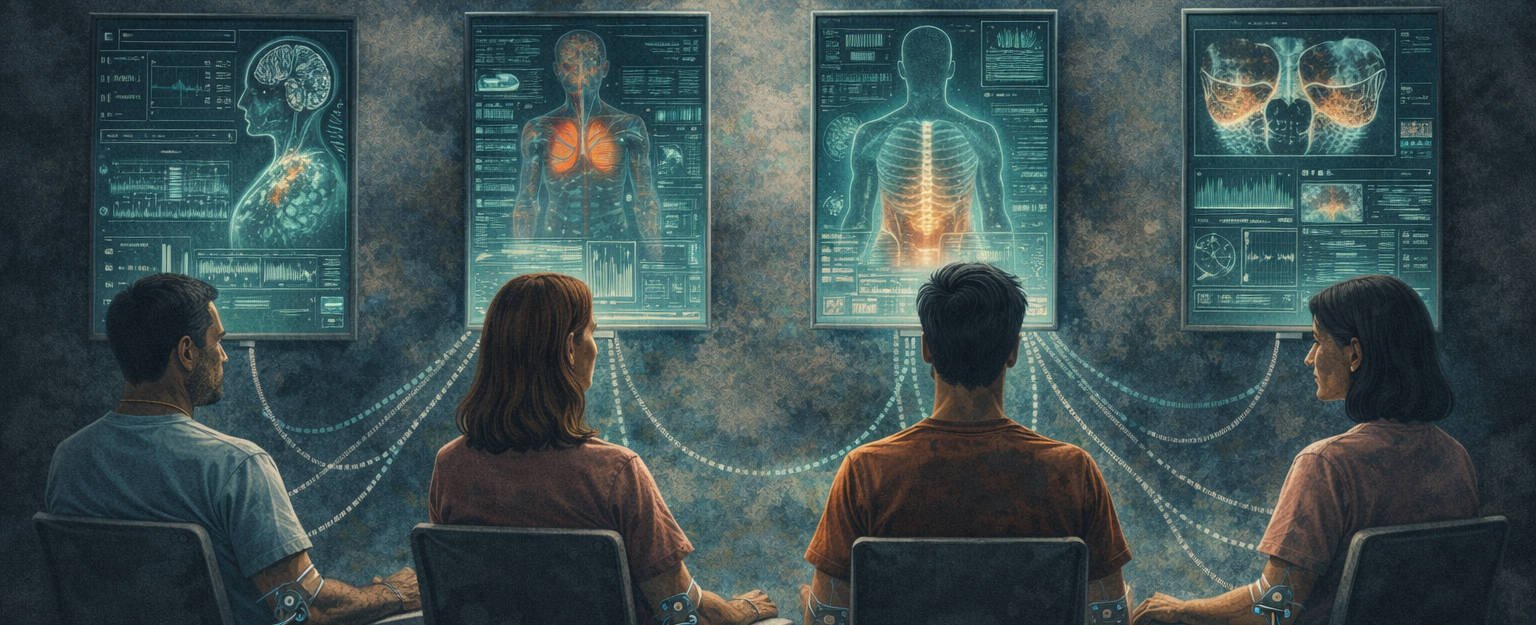
From a patient’s perspective, that gap becomes your responsibility. You become the connective tissue between institutions. You carry context across systems that were never designed to share it. What should feel seamless instead adds friction at moments when capacity is already stretched thin.
If these tools were built around patients first, the data would move with them. Instead, it remains anchored to organizations.
Vulnerability changes the stakes
As a patient, I never believed my correspondence or records were visible beyond my care team. I assumed that safeguards, identifiers, and regulations meant my information stayed where it belonged. Insurance billing felt like an understood necessity, not a risk.
That assumption held until it didn’t.
Learning about recent patient portal data exposure wasn’t alarming because of technical details. It was unsettling because it challenged a basic expectation: that healthcare systems operate under a different moral contract than consumer platforms.
When you’re immunocompromised, exhausted, and navigating treatment during a pandemic, you don’t have the option to interrogate infrastructure. You comply because access to care depends on it.
COVID made that reality more visible. Checking in on my phone before entering a facility felt impersonal, but it made sense. Limiting contact was necessary. What mattered was that once I arrived, the human support was there. Staff helped me navigate unfamiliar buildings. People noticed when I was struggling.
Technology works when it supports care. It becomes a problem when it quietly distances responsibility.
When purpose erodes
I’ve seen what happens when organizations drift away from why they exist.
In fintech, we often pointed to Wells Fargo as an example of how internal incentives can distort judgment. The failure wasn’t a single decision. It was a gradual acceptance of behavior that no longer aligned with stated values. Over time, that self-deception became cultural.
At Kasasa, we tried to guard against that. We talked openly about trust. We built products with flexibility. We drew lines we wouldn’t cross, even if the numbers suggested otherwise. The goal wasn’t to win quarters. It was to serve people well enough that trust compounded over time.
Healthcare isn’t banking, but it isn’t immune to the same pressures. As systems scale, stewardship can give way to optimization. When that happens, patients feel it first.
What changes when patients have agency
During treatment, the most helpful thing I had wasn’t another dashboard. It was the ability to notice patterns and bring them into conversations with my doctors.
Sometimes that backfired. I tracked my heart rate obsessively on my watch, charting the effects of chemotherapy on my body. Eventually, my doctors asked me to stop. The data lacked context. The device didn’t know I had cancer. It only knew deviation from baseline. The alerts added anxiety without insight.
That experience mattered. It reminded me that more data isn’t always better. Tools need context, not constant measurement.
Other times, tracking made a real difference.
When a lumbar puncture went wrong and had to be repeated multiple times, I documented the aftermath: pain, ringing in my ears, numbness in my hands. I connected symptoms to a specific procedure and brought that clarity back to my care team.
When I began experiencing frequent, severe nosebleeds—sometimes so intense they caused me to black out—I started tracking them. Frequency. Duration. Severity. Location. I drew diagrams. I looked for patterns. That record changed the conversation. It gave my symptoms shape.
When patients are able to do this, something shifts. Conversations improve. Decisions become more grounded. Care becomes collaborative.
What breaks first
What breaks first isn’t technology. It’s understanding.
I felt this during scheduling at MD Anderson. I traveled from Austin to Houston expecting a two-day consultation. When additional days were added without acknowledging the impact on work, family, finances, I felt destabilized. The system optimized for availability, not context.
That disconnect isn’t malicious. It’s structural. Analytics and efficiency work well until they lose sight of the person moving through them.
Why Symptom Keep exists
Symptom Keep isn’t designed to replace institutional systems. It’s designed to sit alongside them.
It gives patients a way to track their own experience, in their own words, on their own terms. It helps organize symptoms into something meaningful before they enter the clinical setting. It’s slower by design. Less extractive. Focused on clarity rather than scale.
Patients define what they’re feeling. They describe it. They rate it. The system helps structure that information so conversations with clinicians are more precise, not more overwhelming.
That kind of agency changes the dynamic. Patients aren’t just responding to care. They’re participating in it.
Vigilance as participation
Putting patients at the center changes how healthcare functions. People stop being abstracted into data flows. Systems are held to a higher standard. Trust becomes something that’s maintained, not assumed.
Vigilance isn’t suspicion. It’s attentiveness. It’s staying engaged without surrendering agency.
That’s where Part I leaves off. And it’s where this work continues.
When patients are treated as humans first, care becomes something we build together, even when certainty remains out of reach.

Leave a Reply